Pain rests at the center of nursing practice regularly than lots of people recognize. On a medical ward after 7 p.m., a youngster with a lower arm crack will certainly not look at the IV pump or the actors, they will enjoy your face for hints that things are going to be all right. In an aged care facility, the resident who quit strolling last month might have poorly recognized neuropathic pain. In a hectic emergency situation department, a paramedic handover for a crush injury depends upon just how quickly and safely you can titrate analgesia. The capability that underpins those moments is learnable, improvable, and certifiable, and nurses who invest in organized discomfort administration training normally feel the distinction by the following shift.
This short article unboxes what high‑quality discomfort education looks like for registered nurses, exactly how certification programs develop capability, and where a brief training course can genuinely change method. It likewise discusses how unit codes like PUAEme008 associate with emergency pain expertises, and just how the ideal discomfort monitoring qualification training course advantages not just registered nurses however physio therapists, paramedics, and interprofessional teams.
What competence hurting administration truly means
Competence is not a solitary ability, it is a mix of knowledge, judgment, and execution under pressure. When I advisor early‑career registered nurses, I look for five capacities that signal real discomfort administration competence.
First, precise evaluation. This exceeds asking "what is your pain from zero to 10." It implies selecting the ideal tool for the circumstance, such as a Numeric Score Scale for a lucid grownup, the Wong‑Baker deals with scale for a kid, or the Abbey Discomfort Range for an individual with sophisticated dementia. It suggests acknowledging the restrictions of vital indications as discomfort proxies and correlating the tale with the examination.
Second, pharmacologic fluency. Safe, reliable titration of opioids calls for more than "begin low, go slow-moving." It needs comprehending equianalgesic dosing, the distinction between hydrophilic and lipophilic opioids, ceiling effects for tramadol or tapentadol, and just how renal or hepatic impairment changes your options. It additionally implies being comfortable with accessories like ketamine for opioid‑tolerant clients, or clonidine as component of a multimodal strategy, while expecting hypotension or bradycardia.
Third, non‑pharmacologic strategy and timing. Registered nurses manage the atmosphere and the procedure around discomfort. The peaceful area, the cozy covering, the splint placed before the transfer, the ice prior to the swelling heights, the cognitive reframing during clothing modifications-- these are not niceties; they are evidence‑based analgesic interventions.
Fourth, danger acknowledgment. High‑risk scenarios have patterns: the hypoxic COPD individual with IV morphine; the sickly individual with a femoral fracture and borderline high blood pressure; the patient on high‑dose methadone for opioid usage condition presenting with severe abdominal pain. Skills suggests preparing for respiratory system clinical depression, delirium, or withdrawal, aligning monitoring and rescue medications, and understanding when to escalate.
Fifth, interaction and paperwork. Clear discomfort strategies alter end results. When the analgesic ladder is set out in the notes with targets, intervals, and rescue thresholds, handovers are safer and clients report far better complete satisfaction and function. Pain is a signs and symptom, yet it is additionally a data stream. Proficiency implies reading it and composing it down in a manner coworkers can act on.
Formal discomfort management training programs that result in a discomfort management certification ought to purposefully build these five pillars, not simply lecture on the WHO ladder.
Where certificate programs fit and why they help
On the‑job learning matters, however it leaves spaces. A certificate course hurting management, specifically one designed for nurses, places framework around the art and provides common language throughout a team. The best pain monitoring training programs incorporate pre‑reading, case‑based workshops, simulation with responses, and evaluation connected to competency frameworks.
The roi appears promptly. Medicine errors decline. Patient‑controlled analgesia comes to be much less frightening for personnel and much safer for clients. Nurses really feel more confident setup assumptions with families, like discussing that the goal is improved feature and rest, not complete removal of discomfort, which non‑drug measures are not optional add‑ons. For managers, a discomfort monitoring certification training course supplies evidence for credentialing and meets proceeding expert development demands in such a way that touches daily care.
Programs differ in size. Short programs hurting management might run 4 to 8 hours and focus on assessment tools, multimodal basics, and usual risks. Longer discomfort administration qualification courses cross a number of weeks with self‑paced modules on pathophysiology, opioid stewardship, neuropathic pain, and intricate scenarios like burns or sickle cell crisis. Both have a place. Brief focused training suits a ward rollout or refresher course. A thorough certificate fits a nurse taking on a pain source function, an educator, or a person working in high‑acuity or specialty settings.
The emergency situation context and PUAEme008
Emergency pain administration is a discipline of its own, with speed, unpredictability, and crowded rooms. Prehospital and ED teams need durable training that mixes rapid analysis, protocol‑driven pharmacology, and handbook methods that acquire time prior to clear-cut treatment. In several curricula, you will see system codes like PUAEme008 connected with emergency expertises. In some jurisdictions, PUAEme008 Provide Pain Management defines the abilities and knowledge called for to assess pain, choose proper non‑pharmacological and medicinal strategies, provide or help with analgesics under professional administration, keep an eye on the person, and turn over treatment effectively.
If your company referrals PUAEme008 offer discomfort monitoring, validate the existing variation and regional extent, as unit codes and evidence demands can alter with training bundle updates. In method, a PUAEme008 offer discomfort monitoring program should cover:
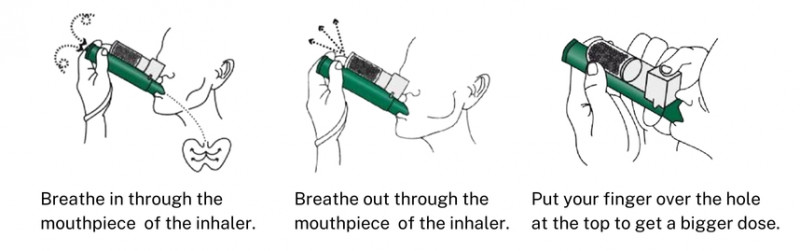
- Rapid pain evaluation in noisy, time‑limited atmospheres, with choices for non‑verbal patients. Indications, dosages, contraindications, and monitoring for generally made use of representatives in the area or ED triage, such as methoxyflurane, intranasal fentanyl, laughing gas, and oral analgesics. Splinting, placing, and cooling down or warming up methods that materially decrease pain before analgesia. Safety methods, consisting of oxygen usage with inhaled representatives, delirium threat in older adults, and documentation that sets the getting collaborate for smooth continuation of care.
When straightened well, a PUAEme008‑based brief course incorporates smoothly right into ED induction and paramedic upskilling and uses a defensible criterion for proficiency sign‑off.
Building blocks of reliable nurse pain education
The ideal pain monitoring programs for nurses share usual functions also when delivered in various formats. First, they adjust web content to the scientific setting. A surgical ward does not require the exact same situations as a pediatric oncology system, and a country ED with limited imaging and postponed transfers has various risk points than a metropolitan trauma center.
Second, they make use of instances, not just slides. I keep in mind a situation made use of in our training that followed an opioid‑naïve postpartum female who established respiratory system clinical depression after repeat IV morphine boluses for incision discomfort. The team needed to map a much safer plan that used scheduled nonsteroidals, local block assessment, and nurse‑activated naloxone parameters. That single instance changed just how several people created post‑cesarean orders for years.
Third, they measure skills with useful jobs. Can you establish PCA with the right lockout and paper sedation ratings properly? Can you chat a patient through utilizing a FACES range when English is not their mother tongue? Can you identify neuropathic functions in an individual with diabetic issues and adjust the strategy accordingly? Observation checklists defeat multiple‑choice alone.
Fourth, they acknowledge predisposition. Research studies reveal that person demographics influence pain ratings and therapy decisions in methods we would rather not confess. Good courses compel representation and offer scripts that standardize treatment, which reduces disparities.
Fifth, they map to credentialing. A discomfort monitoring certification that states which competencies were examined, and at what requirement, is better than a certificate of presence. Nurses deserve acknowledgment that equates to roles and pay, not simply a line in a portfolio.
Pharmacology that nurses in fact use
Every registered nurse who finishes a pain administration certification course need to come away with a sensible, nuanced grasp of anesthetics in genuine settings. That includes recognizing when to choose dental over IV, how to pre‑empt discomfort with regular application, and how to pivot when the initial effort fails.
Nonsteroidal anti‑inflammatory medications lower prostaglandin production and are specifically helpful after orthopedic and oral procedures. The trade‑off is kidney perfusion and bleeding danger, particularly in older grownups and those on anticoagulants. Acetaminophen is a backbone drug, but its ceiling dose matters, and we regularly locate replicate therapy when a patient gets a combination opioid tablet computer plus routine paracetamol.

Opioids remain required in modest to extreme acute pain. Experienced titration is not a guessing game. For IV morphine, initial boluses of 2 to 2.5 mg with reassessment every 5 to 10 mins provide great control. If the person is opioid forgiving, the increments and ceiling shift, yet the concept holds. For intranasal fentanyl, common ED dosages are 1.5 micrograms per kilogram as much as institutional optimums, with repeat dosing based on impact. A pain administration course must infuse respect for opioid kinetics, cross‑tolerance, and the useful use sedation scales like Pasero or RASS as guardrails.
Adjuvants change lives in neuropathic pain. Gabapentinoids, tricyclics, SNRIs, and topical agents like lidocaine spots can be crucial, yet they lug adverse effects that nurses should keep an eye on and clarify. Topical NSAIDs aid in local bone and joint discomfort without system‑wide direct exposure. For intricate acute pain, low‑dose ketamine infusions under protocol, or alpha‑2 agonists, can decrease opioid dosage. Nurses are the ones who discover the very early tremblings of delirium or the creeping blood pressure decline and act before it becomes an accident call.
Regional anesthesia is its own universe, yet every nurse must know with usual blocks in their system, from adductor canal blocks in knee surgical procedure to fascia iliaca blocks in hip fractures. Recognition of anesthetic systemic poisoning belongs to safety and security training, as is accessibility to intralipid protocols.
Non drug methods that really make a dent
Skeptics occasionally dismiss non‑pharmacologic treatments as soft medication, yet they work when delivered with intent. Appropriate limb altitude and compression lower edema and nociceptor activation. Splinting a broken rib with a pillow during coughing, and teaching paced breathing, can transform a person's day. Heat decreases muscle mass spasm; chilly minimizes swelling; both require timing and skin checks.
Cognitive treatments are not the sole purview of psychologists. Basing strategies throughout dressing changes, straightforward led images, and mentoring that reframes pain as a controllable signal, not a tidal bore, boost analgesic feedback. For pediatric people, play therapy and disturbance exceed another IV bolus in particular treatments. Rest is analgesic, sound is the adversary, and registered nurses are the designers of both.
Physiotherapists are vital partners. Discomfort management training courses for physiotherapists usually highlight graded puaeme008 direct exposure, pacing, and practical objectives. When nurses and physio therapists straighten language and timing, individuals set in motion sooner with less distress. Interprofessional brief programs suffering management build this common technique and lower blended messages.
Recognizing and managing special populations
Older adults metabolize medicines differently, and their brains are susceptible to delirium. A secure plan typically begins with scheduled acetaminophen, cautious NSAID use if kidney feature enables, low starting doses of opioids with tight review, and aggressive non‑drug steps. I have seen older patients with hip fractures reverse simply from a fascia iliaca block plus warm coverings, gentle positioning, and regular mentoring to breathe and move.
People with opioid use problem provide an acquainted challenge. Under‑treating their acute pain due to preconception or fear leads to rise habits, inadequate results, and conflict. The much better course is coordination with addiction solutions, continuation of methadone or buprenorphine when feasible, enhancement of greater opioid doses to overcome tolerance in the short term, and clear prepare for taper. Programs that consist of these situations boost personnel convenience and individual trust.
In pediatric setups, dosage arrays are weight‑based and courses matter. Intranasal analgesia radiates here. Educating moms and dads how to use FACES or FLACC scores and what to get out of multimodal analgesia brings them into the team. A discomfort monitoring training program that includes pediatric modules pays for itself the following school holiday season when damaged arms fill the waiting room.
For patients with communication barriers or cognitive problems, confirmed empirical tools like PAINAD or Abbey are essential. Personnel need to recognize the risks, like misreading uneasyness from urinary system retention as discomfort, or missing out on discomfort that presents as withdrawal or reduced activity.
Assessment and documents that individuals can use
Documentation is not a bureaucratic workout. Great notes develop connection. The very best discomfort strategies have clear targets, such as "Goal: pain ≤ 4 at remainder, ≤ 6 on movement; individual able to remain of bed for meals." They define time‑bound actions: "If pain stays ≥ 7 thirty minutes after 2 mg IV morphine, carry out added 1 mg every 5 to 10 mins to an optimum of 6 mg, reassessing sedation with Pasero scale." They advise the next registered nurse of risks: "Display for breathing price << 10 per minute; if occurs, stop opioid and call medical police officer; think about naloxone 40 micrograms IV increments." They detail non‑drug procedures currently attempted and the person's response, so coworkers do not duplicate failures.</p>
Pain reassessment timing varies by path and agent. After oral analgesia, reassess in 45 to 60 minutes. After IV bolus, reassess in 5 to 10 minutes. After local anesthesia, reassess feeling and electric motor function per protocol. Several wards fail at the reassessment action. A pain monitoring certificate program that drills the timing and the why will stop the relentless cycle of "provided something, went on, failed to remember to examine."
Course selection: what to look for
There is no scarcity of programs marketed as pain management training courses for registered nurses. Quality differs. A comprehensive analysis conserves time and prevents stress. Seek external positioning with identified frameworks, such as national discomfort cultures or proficiency criteria utilized in your country. Take a look at the deepness of material beyond the essentials. Does the course enter into opioid conversion, ecstasy prevention, and regional anesthetic security, or does it quit at acetaminophen plus morphine?
Ask about assessment. A pain management certification that needs a case write‑up, a simulated situation, and a racked up monitoring of practice lugs more weight than one that uses just online quizzes. Inspect the professors. Programs instructed by a mix of registered nurses, anesthetists, discomfort medical professionals, and physio therapists bring broader perspectives and even more realistic cases.
Flexibility matters in nursing schedules. The most effective pain administration training for nurses provides modular online theory with short in‑person skills sessions and neighborhood mentors for proficiency sign‑off. If your organization needs an emergency situation focus, focus on suppliers that can supply an emergency discomfort monitoring component or a PUAEme008 provide pain management training course pathway.
Costs vary widely. A half‑day short training course may set you back much less than a change of overtime. A complete discomfort administration accreditation program with evaluation, responses, and a recognized certification will certainly set you back even more and might be eligible for specialist development funding. When budget plans are tight, educate a staff of discomfort champs who can mentor others on the floor.
Implementation lessons from genuine wards
I have actually turned out discomfort education on surgical and medical devices, and the very same useful lessons show up each time. Beginning with the data from your own service. Pull five recent graphes where pain management went poorly and anonymize them for discussion. Staff engagement increases when the cases look acquainted. Mix fast success with deeper modification. Quick wins consist of systematizing discomfort scales by person team, uploading rescue application algorithms at medicine terminals, and making cold pack and warmth packs easy to find.
Deeper change involves order collections and protocols. Collaborate with prescribers to standardize multimodal pre‑emptive analgesia for usual procedures and to embed reassessment timing prompts in electronic documents. Identify 1 or 2 registered nurses per shift as pain resources who can be called for suggestions. Display for unintended effects, such as a rise in constipation from far better opioid initiation, and respond with automated digestive tract routines and patient education leaflets.
Measure what matters. Numerical pain scores are just component of the image. Track useful outcomes: time to initial mobilization, ability to sleep through the night, involvement in physiotherapy. Share tales of success and near misses out on in huddles. A discomfort administration training pain management certification course program sticks when it becomes part of the system's language.
Interprofessional advantage, not simply nursing
Although this write-up concentrates on pain monitoring training for nurses, the best programs explicitly invite physio therapists, pharmacologists, and junior medical professionals. Discomfort monitoring training courses for physio therapists highlight graded exposure and activity strategies that depend on worked with analgesia. Pharmacologists add necessary roughness to medication settlement and adjustments for renal or hepatic disability. When groups educate with each other, you obtain faster PCA troubleshooting, better pre‑op counseling, and fewer blended messages to clients like "remain in bed" from a single person and "set in motion per hour" from another.
For ED and prehospital solutions, interprofessional training is not optional. A paramedic with a PUAEme008 history and an ED nurse with a strong pain management certification structure will certainly turn over and proceed care seamlessly, minimizing replication and delay.
Certification versus competency: making both count
A discomfort administration certificate signifies training course conclusion. Competency suggests you can do the job to standard under genuine conditions. The goal is both. Programs need to supply the certificate and an expertise checklist linked to evident behaviors: appropriate use of discomfort scales, proper medicine option and titration, risk-free surveillance, reliable non‑pharmacologic treatments, and clear documentation.
Managers can make use of these checklists for neighborhood sign‑off, tied to benefits like hanging ketamine infusions, starting nurse‑driven analgesia procedures, or managing PCAs. Registered nurses can keep them in their portfolios for recredentialing and job applications. Gradually, refresher courses maintain the side. Pain practice modifications: brand-new guidelines for opioid stewardship, brand-new local blocks, far better ecstasy prevention. Set a cycle, typically two to three years, for a pain management qualification program update, with much shorter refresher courses in between.
Two sensible checklists you can utilize tomorrow
- Rapid ED discomfort strategy at triage: 1) Determine most likely pain mechanism and seriousness, 2) Choose a route that works currently, 3) Apply a physical intervention right away, 4) Paper reassessment time, 5) Flag dangers and monitoring needs. Ward based multimodal bundle after major surgery: 1) Arrange non‑opioids around the clock unless contraindicated, 2) Consider regional or local options early, 3) Use low‑dose opioids for innovation with clear ceilings, 4) Mandate reassessment times and sedation scoring, 5) Set analgesia with mobilization and bowel regimen.
These lists are beginning factors, not substitutes for formal training. They function best when woven right into protocols and reinforced during handovers.
Where to go next
If you are a registered nurse mapping your advancement for the coming year, take into consideration a split technique. Start with a brief training course suffering management that fits your existing unit, after that plan for a more comprehensive pain administration accreditation training course within six to twelve months, preferably one that consists of simulation and examined competencies. If your role includes triage or ambulance user interface, look for an emergency situation pain administration component or a PUAEme008 provide discomfort monitoring path acknowledged in your region.
For educators and managers, construct a regional curriculum that blends inner teaching with outside certification. Align it to your medicine formulary, your surveillance devices, and your patient population. Track results, share success, and take another look at material annually.
The work deserves it. When a scared individual kicks back since you described the plan and the strategy functions, when a youngster laughs during a procedure because your distraction techniques landed, when an older adult avoids delirium since your team balanced analgesia and watchfulness, you feel the distinction. Pain administration training for registered nurses is not just a certificate on a wall surface. It is a collection of competencies that change the day for the individual in front of you, and for the registered nurse that wishes to go home recognizing they did right by them.